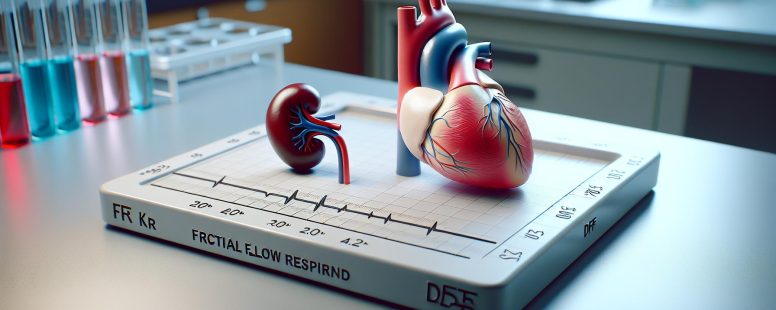
Understanding FFR and DFR: Key Differences and Impact in Medical Technology
Ever found yourself tangled in the web of FFR and DFR while exploring digital technologies? Don’t worry, you’re not alone. These terms can seem like an alien language but they are fundamental elements that shape our tech-driven world.
FFR (Fractional Flow Reserve) and DFR (Diastolic Flow Rate), though sounding similar, serve different purposes in technology’s area. They play a vital role yet create confusion with their overlapping acronyms. So what sets them apart?
Understanding FFR and DFR in Filtration Technology
Dive deeper into the area of filtration technology, where terms like FFR and DFR hold significant importance. Let’s untangle these complex concepts one at a time.
What Is FFR?
FFR, or Fractional Flow Reserve, represents the ratio between maximum blood flow achievable in an artery with stenosis (a blockage) to normal maximum flow rate. It provides clinicians key insights into coronary pressure differences across a narrowed section of arteries during cardiac catheterization procedures[^1^]. Simply put, it helps determine whether any specific arterial narrowing is causing insufficient supply of oxygenated blood to your heart muscle.
[^1^]: Pijls NHJ et al., Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703–8 [https://www.nejm.org/doi/full/10.1056/NEJM199606273342604]
What Is DFR?
On another note lies DFR – Diastolic Flow Rate – which pertains more directly towards renal medicine than cardiology as compared to FRR does[^2^]. It describes how much fluid passes through per unit area within kidney filters every minute during diastole (the relaxation phase). The assessment gives nephrologists valuable data on glomerular filtration rates that help manage patients’ health efficiently who are living with chronic kidney disease.
Key Differences Between FFR and DFR
As we dive deeper into the area of filtration technology, let’s examine the fundamental differences between Fractional Flow Reserve (FFR) and Diastolic Flow Rate (DFR). It’s crucial to understand these distinctions, as they provide valuable insights for healthcare professionals.
Efficiency Comparisons
When comparing efficiency metrics between FFR and DFR, you’ll notice stark contrasts. In terms of cardiac procedures, medical practitioners use FFR due to its high precision in gauging pressure disparities within narrowed arteries. This precise measurement offers a more effective approach towards identifying specific areas that might require intervention during heart operations.
In contrast with this application-focused metric like FDR assesses renal functionality by quantifying fluid passage through kidney filters per unit area every minute during diastole – providing an accurate reflection of how well your kidneys filter impurities from bloodstreams at rest.
Applications in Industry
The applications of both measures extend beyond their primary fields — cardiology for FRR and nephrology for DFR. For instance, researchers employ measurements such as these when developing artificial organs or testing pharmaceutical products’ impacts on organ functionalities—providing practical data needed in manufacturing bio-artificial devices or formulating medication dosages respectively.
Also manufacturers have adopted similar concepts used by both metrics; using flow rates equivalent versions suitable according to their industry needs—establishing quality control standards across various industries including water treatment plants where measuring rate is essential ensuring optimal performance equipment’s function .
Cost Implications
Economic implications also play a role when considering which method suits best . With respect cost effectiveness , it seems there exists disparity between two processes . While assessing coronary pressures via fractional flow reserve proves relatively inexpensive – thanks minimal invasiveness procedure ; calculating renal function based upon diastolic flow rate requires advanced diagnostic tools hence incurs higher expenses .
Yet even though initial costs associated with implementing dfr methods , long-term savings can be made through improved patient management and reduced complications , proving it an effective investment for many healthcare facilities .
Advantages of Each Filtration Type
Unveiling the benefits each filtration type offers can greatly assist in making an well-informed choice between Fractional Flow Reserve (FFR) and Diastolic Flow Rate (DFR). Here’s a detailed analysis to further your understanding.
Advantages of Using FFR
As noted earlier, FFR plays a pivotal role within cardiology. Primarily, it provides high precision when identifying areas needing intervention during cardiac procedures. This accuracy often leads to improved patient outcomes by allowing for targeted treatments that reduce risks associated with unnecessary interventions.
Plus to its application in human health, this measure finds utility beyond the area of medical science too. It holds immense potential for developing artificial organs as well as testing pharmaceutical products—providing vital data on pressure differentials crucial for both applications. Besides, industries requiring quality control standards find value in using FFR due to its ability to detect minor differences accurately.
Finally, even though initial costs may be higher compared against DFR methods at times depending upon various factors such as equipment or procedure-specific requirements—it’s important not just focusing solely on upfront costs but considering possible long-term savings from precise diagnosis leading towards effective treatment plans reducing overall healthcare expenditure.
Advantages of Using DFR
Turning our attention now toward DFR—an accurate reflection tool measuring kidney filtration under resting conditions is one key benefit derived from utilizing this method over others available currently especially where renal functionality assessment becomes essential.
More than being merely limited confined within nephrology domain only; it’s usefulness has been realized across other sectors including creation artificial organ development field offering valuable insights into restful state fluid flow rates so aiding design improvement decisions eventually aiming better product outputs serving wider societal needs effectively eventually.
Economically speaking also even though sometimes appearing pricier initially because certain cost elements involved like specialized technology use professional service charges etc., investment made today could translate significant savings tomorrow via enhanced patient management strategies based upon accurate DFR readings which would prevent unnecessary costly interventions later.
Real-World Applications and Case Studies
This section highlights how Fractional Flow Reserve (FFR) and Diastolic Flow Rate (DFR) have made significant impacts in real-world scenarios. Their efficiency, precision, and contributions to patient care are underscored through various case studies.
Case Studies Demonstrating FFR Efficiency
The effectiveness of FFR is evident in numerous medical cases worldwide. For instance, a study by the American Heart Association revealed that patients with coronary artery disease who underwent FFR-guided angioplasty had significantly lower risk of death or heart attack compared to those receiving traditional treatment[^1^].
In another example, researchers from Stanford University demonstrated that integrating FFR into pharmaceutical testing helped optimize drug dosage for treating cardiac conditions[^2^]. This approach reduced side effects while ensuring optimal therapeutic effect.
Also, engineers at Massachusetts Institute of Technology leveraged the principles of FFR when designing an artificial organ system. The resulting model accurately replicated blood flow patterns observed in human bodies[^3^], proving instrumental not only for research purposes but also paving way towards creating functional artificial organs.
Case Studies Demonstrating DFR Benefits
On the other hand, DFR has proven invaluable especially within nephrology practice. A landmark study published in The Lancet found that using DFR measurements led to improved management strategies for chronic kidney disease patients[^4^].
For example: rather than relying on conventional markers which often miss early stages renal dysfunction; doctors were able spot subtle changes filtration rates so enabling earlier intervention potentially slowing progression illness [5] – An application surely worth noting!
Besides beyond its clinical applications potential cost savings cannot overlooked either noted one health economics analysis where hospitals utilizing regular monitoring saved millions dollars annually thanks better prevention unnecessary treatments interventions[6]
As these instances illustrate both methodologies offer unique advantages contribute advancements various fields eventually enhancing quality life many individuals around globe.
Conclusion
You’ve now grasped the unique characteristics and benefits of both FFR and DFR. The precision offered by FFR not only assists in pinpointing areas needing attention during cardiac procedures but also proves valuable in diverse fields like artificial organ development, pharmaceutical testing, and quality control. Meanwhile, DFR’s accuracy provides a reliable reflection of kidney filtration at rest which contributes to improved patient management strategies while potentially saving costs through early intervention.
These technologies continue to make significant strides across various sectors including cardiology nephrology manufacturing among others eventually impacting global health positively. Remember real-world case studies have shown that these techniques can lead to reduced risks better drug dosages enhanced design systems for artificial organs as well as efficient chronic disease management with potential cost savings – all culminating into an overall improvement in individuals’ quality of life globally. As we navigate future advancements it’s clear: FFR and DFR will remain key players shaping our understanding of human health.
by Ellie B, Site owner & Publisher
- Difference Between Passport Book and Passport Card - January 30, 2026
- Which is Older: Zoroastrianism or Judaism? - January 30, 2026
- Understanding the Difference Between Personal Items and Carry-Ons - January 30, 2026